In Opioid Guidelines We Trust?
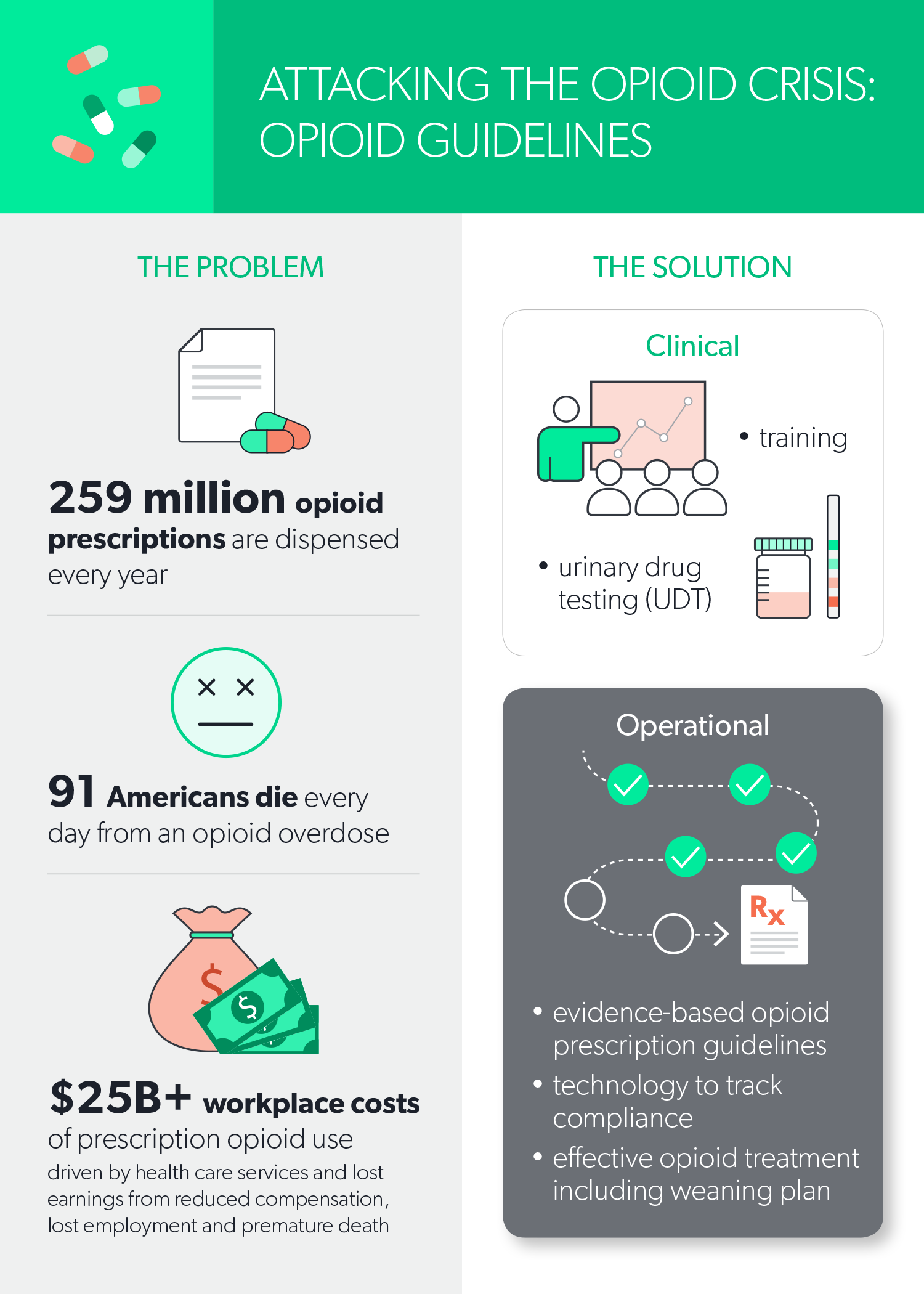
A common recommendation to combat the current opioid epidemic is to provide physicians with opioid prescribing guidelines. Opioid guidelines synthesize the available research to inform judicious prescribing behaviors and safe dosages when opioids are needed. Given the seriousness of the opioid epidemic, it is not surprising that multiple organizations currently produce opioid prescribing guidelines. Opioid guidelines are based on evaluations of the research, but the guidelines themselves need to be evaluated critically, as well.
Guideline Evaluation
Fortunately, there are multiple standards currently available to evaluate guidelines, including AGREE (Appraisal of Guidelines, Research and Evaluation), IOM (Institute of Medicine), GRADE (Grading of Recommendations Assessment, Development and Evaluation) and AMSTAR (A Measurement Tool to Assess Systematic Reviews). For example, the AGREE consortium’s latest standard (AGREE II) provides a 23-point checklist covering six domains: scope and purpose, stakeholder involvement, rigor of development, clarity of presentation, applicability and editorial independence. While some AGREE II domains are obvious criteria including “rigor of development” and “editorial independence,” other domains such as “applicability” are less obvious but important. For example, one part of “applicability” is about providing advice or tools for translating recommendations into practice. This point is important considering opioid prescribing guidelines will only work if practitioners can integrate use of the guidelines into their workflow and can apply them effectively to the appropriate individuals. Most chronic opioid users’ first exposure to opioids is through a physician’s prescription, and physicians’ opioid-prescribing patterns have been shown to be associated with opioid abuse and deaths. Therefore, preventing unnecessary first exposure to opioids is crucial.
Guideline standards have shown that not all opioid treatment guidelines are of equal quality. For example, Nuckols et al. (2014) assessed 13 opioid guidelines using the AGREE II and AMSTAR instruments. The authors found AGREE II scores ranged from 3.00 to 6.20 on a 1 to 7 scale, and AMSTAR ratings ranged from poor to high. Four of the guidelines were “recommended against using … because of limited confidence in development methods, lack of evidence summaries or concerns about readability.” This research proves that the quality of opioid guidelines does vary.
The National Guidelines Clearinghouse (www.guideline.gov) is a publicly available resource that provides summaries of guidelines that comply with IOM standards. Although not all guidelines are available free on the National Guidelines Clearinghouse website, it could be a good starting point for finding organizations with guidelines that adhere to a guideline standard.
Jim Smith’s Story
Jim Smith’s occupational injury provides a useful example of how being prescribed opioids contrary to high-quality treatment recommendations may lead to serious health and economic consequences. Jim is a 38-year-old construction worker who suffered an extremely painful lower back strain while attempting to lift a heavy box. Against most guidelines’ recommendations, he was treated from the start with a long-acting opioid, on which he became first dependent and then addicted, taking increasingly higher doses. Even on doses exceeding most guidelines’ recommendations, Jim still suffered from pain and limited mobility. In addition, he began to require supplemental medication to treat the side effects of his opioid use, such as constipation. He subsequently underwent surgery on his lumbar spine, which did not provide him relief from his pain, and he ended up a chronic user of opioids, permanently disabled and housebound.
If Jim had been treated according to any of the current, high-quality opioid treatment guidelines, he would not have received a prescription for an opioid as an initial measure. He would have been counseled to try over-the-counter medications such as ibuprofen or acetaminophen, sent to physical therapy, prescribed exercise and perhaps offered a course in cognitive behavioral therapy (CBT). If opioids had been truly necessary in the acute phase of Jim’s injury, he would have been prescribed a limited course and then been gradually tapered off.
Conclusion
It is very important to find guidelines that both reduce initial use of opioids and serve to guide the physician in tapering chronic opioid users off these drugs. For someone who has been on opioids for a long time, the tapering process could take many months or years, and there could be both physical and psychological complications during the taper. The process for weaning someone off chronic opioid usage will be discussed in the next article in this series.
In conclusion, users of treatment guidelines put a lot of trust into the recommendations provided. Using only opioid treatment guidelines with sound quality and content helps keep that vital trust so clinicians can continue to use guidelines in combating the prescription opioid epidemic.