Products
CLARA Fraud
Identify Suspicious Medical & Legal Activity
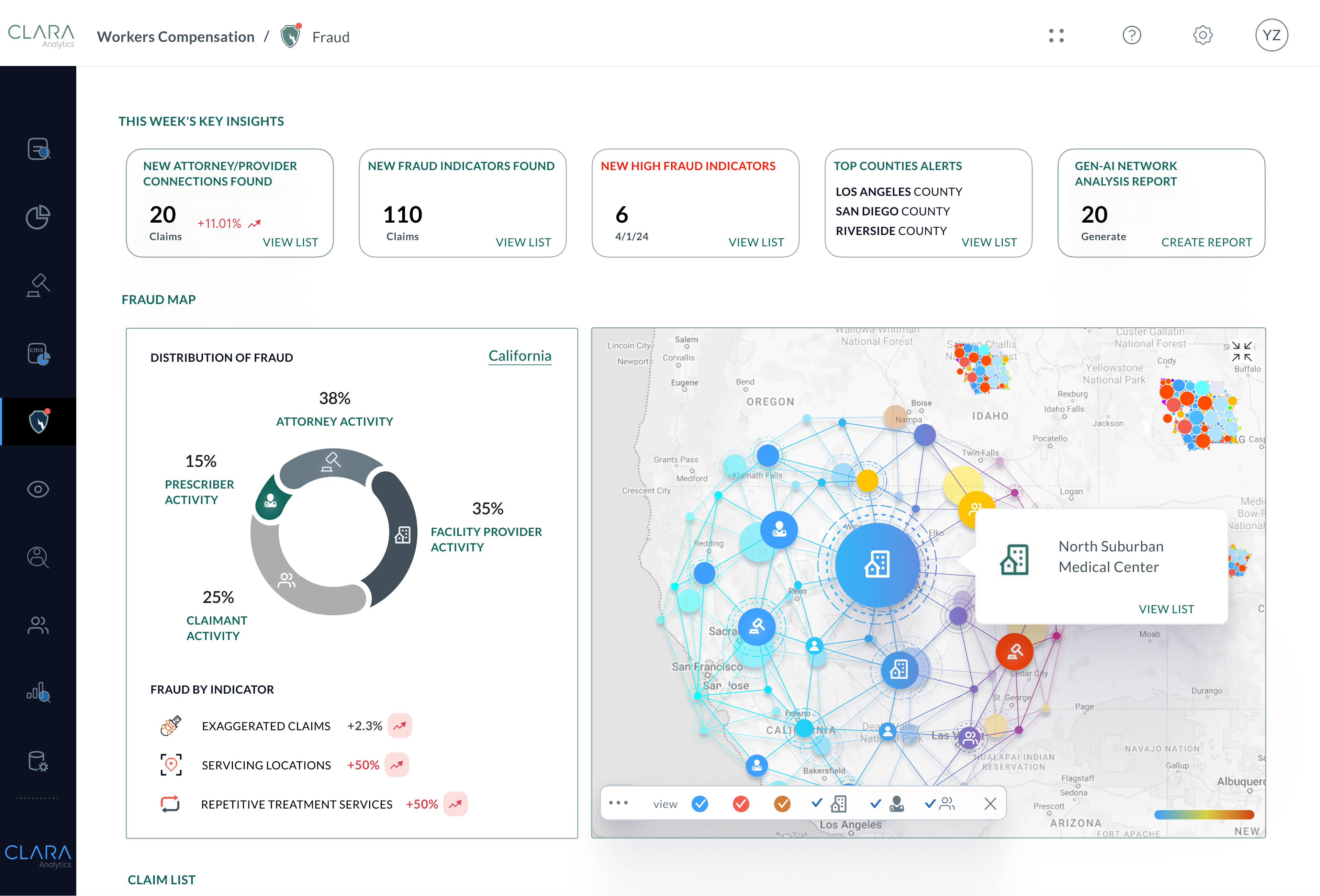
CLARA Fraud uses AI fraud prevention to help identify suspicious activity by examining the relationships between medical providers, legal counsel and claimants across millions of workers compensation claims.
Suspected Fraudulent Behavior Insights for SIU Referrals
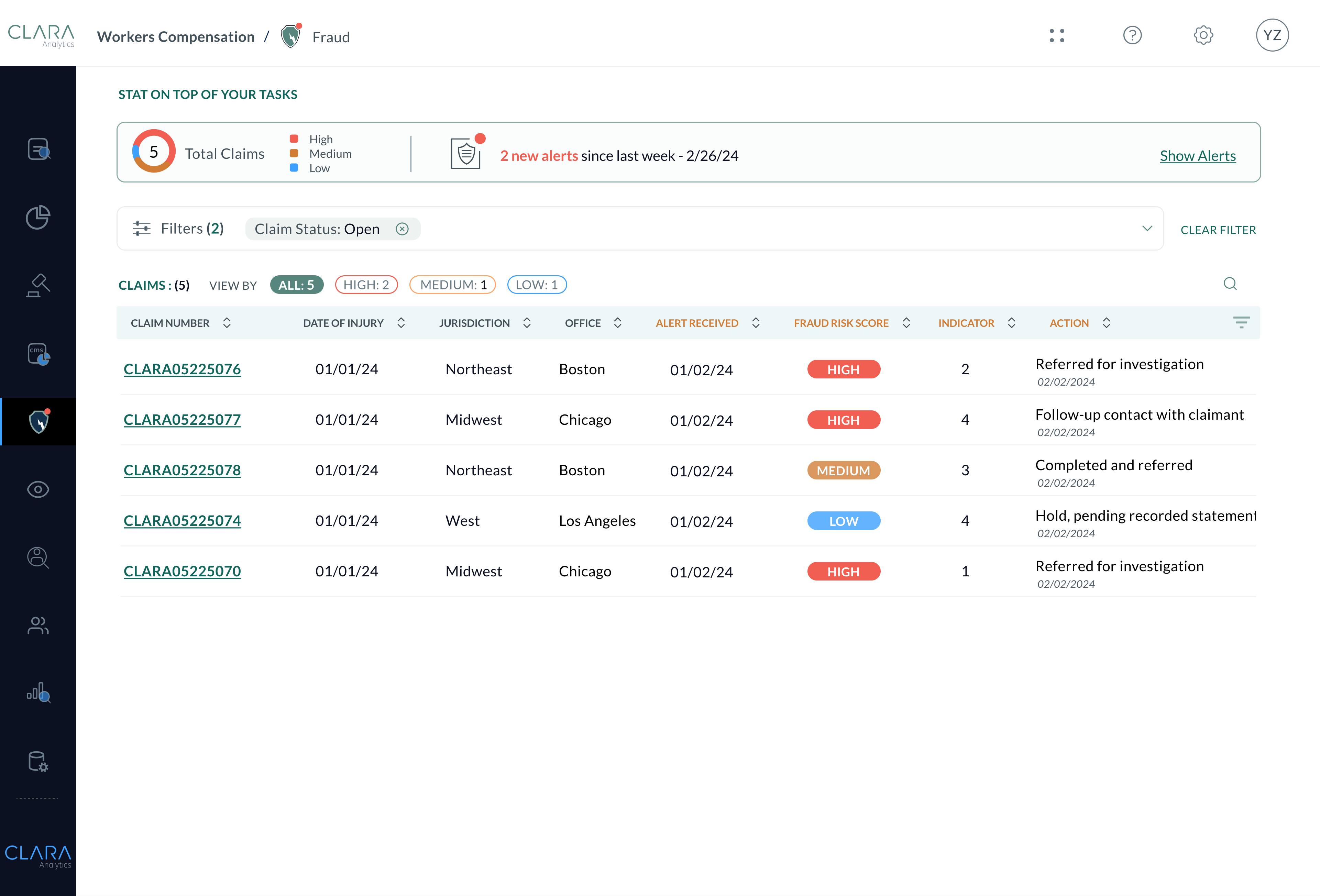
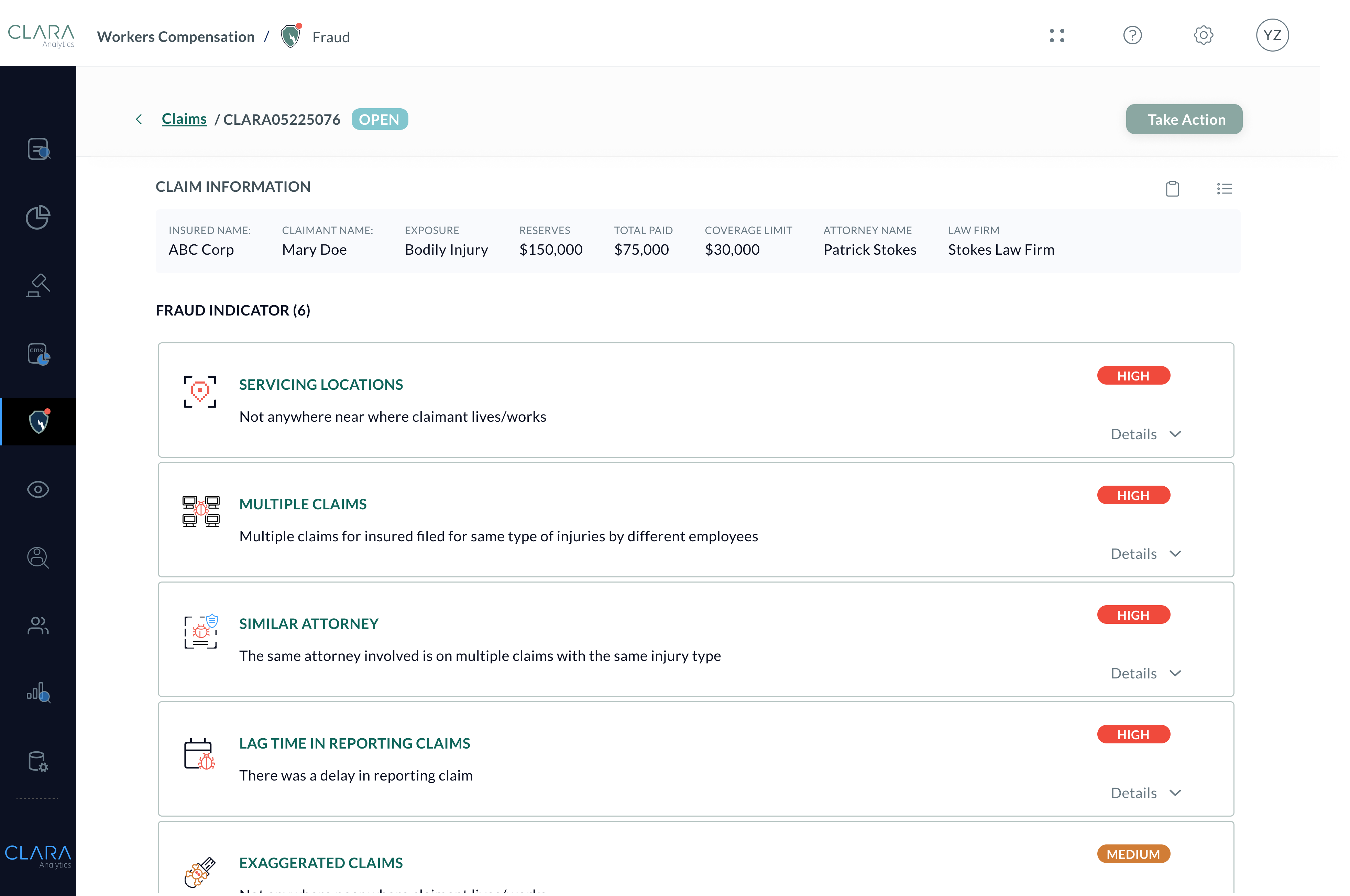
CLARA Fraud analyzes claims data, billing records and legal demands using fraud risk scoring to alert and provide justification for SIU referrals. Eliminate false positives and uncover fraudulent activity from bad actors across millions of claims.
Download product sheet Identify Suspicious Activity Invisible to the Human Eye
Humans cannot keep tabs on every attorney, medical provider, and claimant, making it virtually impossible to examine the vast number of cases needed to identify patterns of fraud. Let AI-powered fraud risk scoring and claims fraud analysis tools do this for you.
Augmented Intelligence Learns from Millions of Claims
CLARA Fraud adds a second set of eyes on all of your claims by alerting on cumulative fraud indicators across all claims on the CLARA platform. Let AI expose fraud patterns that even the most senior adjuster could miss.
Stop Bad Actors Quickly and Confidently
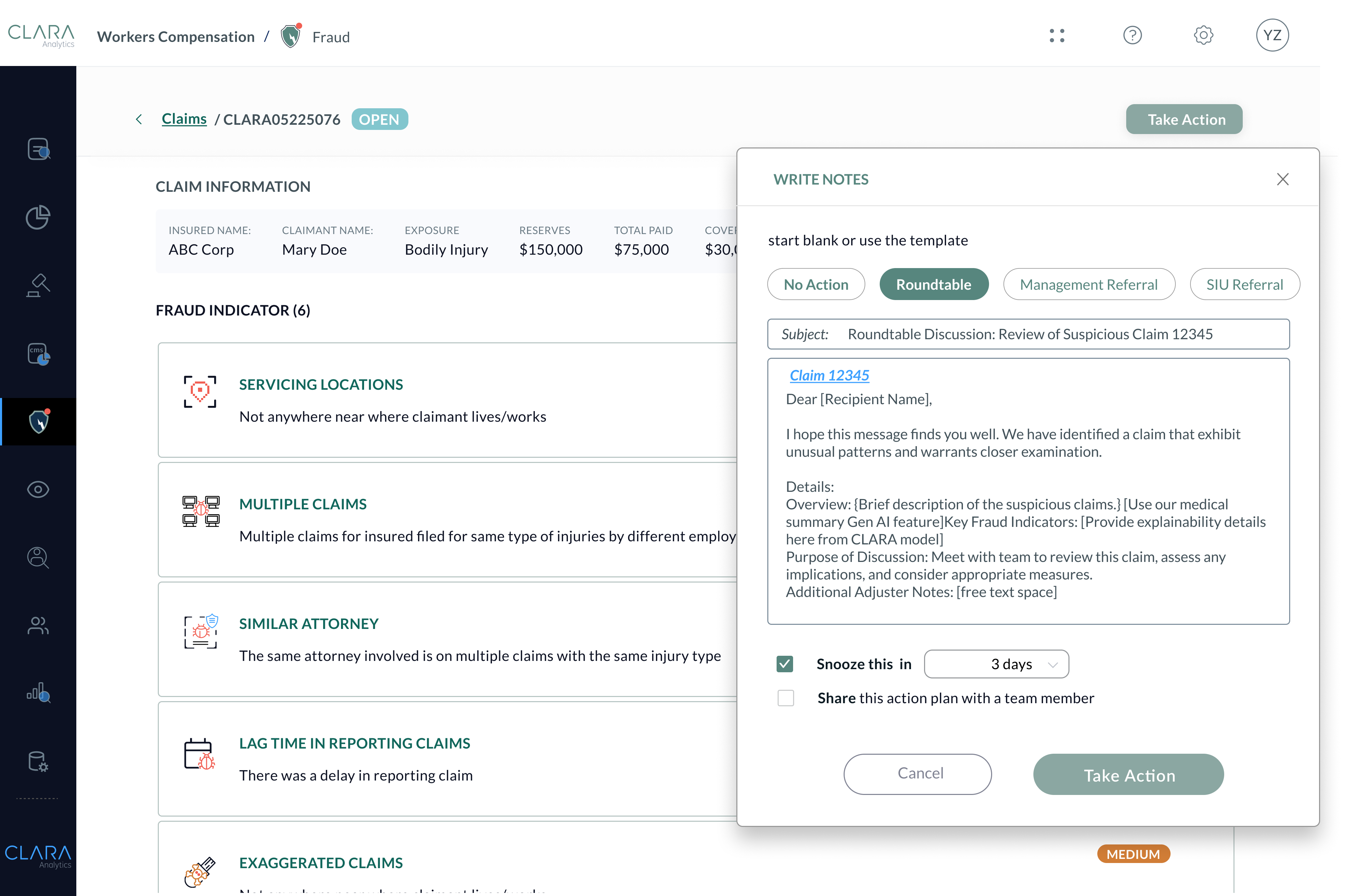
Anyone handling a claim can benefit from CLARA Fraud’s speed and accuracy. Feel confident in your SIU and claims management referrals, avoid false positives, and avoid unnecessary loss costs. Use AI-driven fraud detection to justify investigation referrals and stop bad actors.
1 1
Key Benefits
- Identifying Systemic Fraud Across Workers Compensation Claims with AI Fraud Prevention
- Streamline SIU referrals with data-informed justification
2 2
The Result?
- Improved referral acceptance rate
- Lower claim operational costs
- Optimized claim outcomes
3 3
Ideal For
- Investigative Units
- Roundtable Teams
- Claims Adjusters
- Legal Teams
Detect systemic patterns of suspicious behavior

CLARA Fraud deploys in weeks with little IT effort
CLARA Fraud has the flexibility to integrate with you
CLARA Fraud is secure with annual certifications
Easy to Deploy
Our cloud-based platform can be up and running in 8-12 weeks after historical data is received, including model tuning, alert configuration, and hands-on training for adjusters.
Seamless Workflows
Adjusters can access claims directly via our cloud-based module at any time from any location, or flex their existing systems with our pre-built APIs for simple integration.
Security is our Priority
Rest easy with HIPAA compliance, annual SOC 2 certification, and data encryption that meets or exceeds industry standards in safeguarding your data.